
In some patients in whom a colonoscopy is contraindicated, however, a CTVC is a reasonable alternative, as the sensitivity for identifying lesions larger than 10 mm is over 90%. 2 Colonoscopy is preferable to a computed tomography virtual colonoscopy (CTVC) to investigate IDA as it can detect superficial lesions such as angiodysplasia. Positive findings on a colonoscopy, which can account for IDA include: malignancy, polyps, angiodysplasia or inflammatory bowel disease (IBD). If a patient has significant comorbidities, endoscopic procedures may be too risky and may not alter patient management, and so these examinations should not be performed. Currently, however, there is insufficient evidence to recommend its use in symptomatic patients and it should be confined to the screening population.ĭual pathology can be found in 1–10% of patients, 1 so it is important that both investigations are performed, even if the first examination finds a cause for the iron deficiency.Įndoscopic investigations should only be performed if the benefit of the procedure outweighs the risk. 11 Faecal immunochemical testing (FIT), an alternative stool test that detects the presence of human globin, has a significantly higher sensitivity and specificity for the detection of colonic neoplasia 12 and may be appropriate as an alternative to FOBt. A meta-analysis of 13 studies looking at the sensitivity of the FOBt in the detection of colorectal cancer (CRC), compared to colonoscopy showed that the sensitivity was 71.2% in the proximal colon and 80.1% in the distal colon. However, in the view of the authors this approach is inappropriate because the low sensitivity of FOBt makes it inadequate for this purpose and significant pathology will be missed.

The use of faecal occult blood testing (FOBt) in the investigation of IDA is recommended by the National Institute for Health and Care Excellence (NICE) as an alternative to endoscopic investigation in patients less than 60 years of age. 1 The presence of associated red-flag symptoms, such as dysphagia or rectal bleeding at any age, should trigger endoscopies via a 2WW pathway. A colonoscopy is indicated in this group only if there are symptoms of lower GI disease or a strong family history of colon cancer. The prevalence of IDA in menstruating women due to menstrual blood loss is high therefore, a gastroscopy is only indicated in this group if symptoms of upper GI disease are present. 6 This failure of release of iron from the ferritin stores results in a low iron, low transferrin saturation and low TIBC, with a high ferritin (Table 1).īSG = British Society of Gastroenterology GI = gastrointestinal OGD = oesophagogastroduodenoscopy NICE = National Institute for Health and Care Excellence 2WW = two-week wait 5 Hepcidin binds to ferroportin (the iron exporter on cells) which results in internalisation and degradation of this transporter, which reduces iron release from cells. 4 Studies have shown that hepcidin expression is upregulated when there is infection or inflammation, via inflammatory cytokines such as IL-6. Mice studies have shown that deletion of the hepcidin gene results in iron overload 3 and, conversely, overexpression of this gene resulted in anaemia. The role of the peptide, hepcidin, in ACD became evident after key studies in 2000 and onwards. In contrast, in anaemia of chronic disease (ACD) the ferritin is raised, owing to an increase in the iron regulator hepcidin.

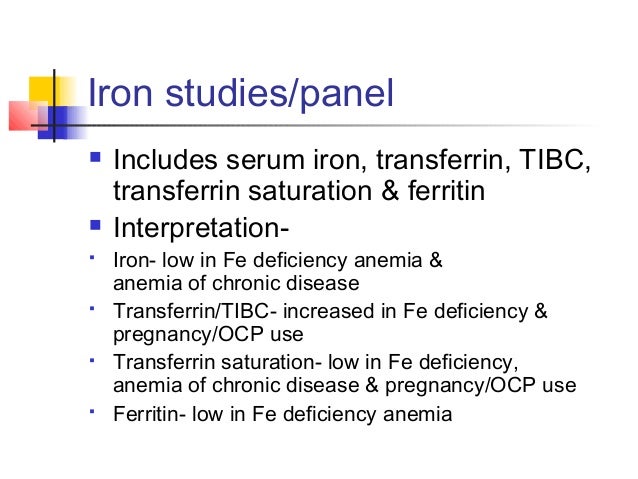
The serum transferrin concentration (expressed in mg/dL) increases in IDA, as the body tries to compensate for low iron levels and this correlates positively with the TIBC. In IDA, the ferritin, serum iron and transferrin saturations are low, but the TIBC increases. The transferrin saturation is the amount of iron that is bound to transferrin, expressed as a percentage of the TIBC. The TIBC (expressed in μg/dL or μmol/dL) is the maximum amount of iron that can be bound by transferrin if this were 100% saturated. In the bloodstream, serum iron is carried bound to transferrin. Iron studies include serum iron level, transferrin saturations and total iron-binding capacity (TIBC) or transferrin concentration, in addition to ferritin.


 0 kommentar(er)
0 kommentar(er)
